NUPLAZID® (pimavanserin) is indicated for the treatment of hallucinations and delusions associated with Parkinson’s disease (PD) psychosis.
NUPLAZID Efficacy Data
Pivotal trial
NUPLAZID significantly reduced the frequency and/or severity of hallucinations and delusions associated with PD psychosis (Primary Endpoint)1
Patients taking NUPLAZID showed signs of improvement as early as Week 2, with significant reductions at Weeks 4 and 61,2


NUPLAZID has been studied in patients with PD-related hallucinations and/or delusions with or without dementia1
In a SAPS-PD responder analysis, 26.3% of NUPLAZID-treated patients experienced a worsening of or no change in their SAPS-PD scores vs 44.4% for placebo.1
Study design: A Phase 3, randomized, double-blind, placebo-controlled, parallel-group study of patients with hallucinations and delusions associated with PD psychosis (N=199). Primary efficacy was evaluated based on change from baseline to Week 6 in the 9-item SAPS-PD total score.1,2
Study population: The mean age of patients enrolled in the clinical study with NUPLAZID was 72 years and patients had MMSE scores ≥21.2 At screening, 20% of patients (40/198) had a history of dementia per medical history, and 37% of patients (69/185) were taking anti-dementia medications at baseline.3,4 The mean SAPS-PD baseline score was 15.9 (6.12) for NUPLAZID and 14.7 (5.55) for placebo.1,2 The majority of patients were on PD medications at entry; these medications were required to be stable for at least 30 days prior to study start and throughout the study.1
Study results: The LSM change from baseline (SE) for NUPLAZID was -5.79 (0.66) and -2.73 (0.67) for placebo; placebo-subtracted difference (drug minus placebo) for NUPLAZID was -3.06 (95% CI: -4.91, -1.20).1 While the primary endpoint was designed to measure change from baseline to Week 6, a statistically significant difference between NUPLAZID and placebo was observed at Week 4 (P=0.0369) and again at Week 6 (P=0.0014).1,2
LSM=least squares mean; SAPS-PD=Scale for the Assessment of Positive Symptoms adapted for Parkinson’s disease; SD=standard deviation; SE=standard error.
Important Safety Information
Contraindication: NUPLAZID is contraindicated in patients with a history of a hypersensitivity reaction to pimavanserin or any of its components. Rash, urticaria, and reactions consistent with angioedema (e.g., tongue swelling, circumoral edema, throat tightness, and dyspnea) have been reported.
NUPLAZID did not impact motor function or activities of daily living vs placebo at Week 6 (Key Secondary Endpoint)1,2
Motor function change from baseline to Week 6 in UPDRS Parts II+III (LSM-SE)1,2


- Mean change from baseline was −1.4 for NUPLAZID (n=92) and −1.7 for placebo (n=88) (placebo-subtracted difference [95% CI] 0.3 [−2.1, 2.7])1,2
- Mean UPDRS Parts II+III baseline score was 51.5 for NUPLAZID and 52.6 for placebo2
- UPDRS Part II is an evaluation of activities of daily living, including speech, handwriting, cutting food and handling utensils, dressing, turning in bed and adjusting bed clothes, and walking7
- UPDRS Part III is a motor exam that includes an evaluation of speech, tremor at rest, rigidity, hand movements, foot agility, and postural stability7
UPDRS Parts II+III=Unified Parkinson’s Disease Rating Scale Parts II and III.
Important Safety Information
Warnings and Precautions: QT Interval Prolongation
-
NUPLAZID prolongs the QT interval. The use of NUPLAZID should be avoided in patients with known QT prolongation or in combination with other drugs known to prolong QT interval (e.g., Class 1A antiarrhythmics, Class 3 antiarrhythmics, certain antipsychotics or antibiotics).
-
NUPLAZID should also be avoided in patients with a history of cardiac arrhythmias, as well as other circumstances that may increase the risk of the occurrence of torsade de pointes and/or sudden death, including symptomatic bradycardia, hypokalemia or hypomagnesemia, and presence of congenital prolongation of the QT interval.
SAPS-PD responder analysis
NUPLAZID responder analysis: Real improvement for the majority of your patients with PD psychosis
About 65% of NUPLAZID-treated patients experienced a clinically meaningful ≥3-point response vs 42.2% for placebo1*


Note: Complete response=SAPS-PD scores reduced to 0 from baseline value. Patients with missing values were counted as nonresponders.1
*Based on regression analysis, a clinically meaningful 1-unit change in the CGI-I scale was associated with a 2.33-point change in SAPS-PD.5
13.7% of NUPLAZID-treated patients experienced complete resolution of symptoms (SAPS-PD score reduced to 0 from baseline) vs 1.1% for placebo.1
26.3% of NUPLAZID-treated patients experienced a worsening of, or no change in their SAPS-PD scores vs 44.4% for placebo.1
Important Safety Information
Drug Interactions:
-
Coadministration with strong CYP3A4 inhibitors increases NUPLAZID exposure. Reduce NUPLAZID dose to 10 mg taken orally as one tablet once daily.
-
Coadministration with strong or moderate CYP3A4 inducers reduces NUPLAZID exposure. Avoid concomitant use of strong or moderate CYP3A4 inducers with NUPLAZID.
Open-label extension
Sustained results over 10 weeks
NUPLAZID efficacy results were sustained, with reductions in the frequency and/or severity of hallucinations and delusions continued from Week 6 through Week 10 in an open-label extension (OLE) of the 6-week, controlled study8*†


*Of the 176 patients who completed the 6-week study, 171 entered the open-label extension (OLE) study, and 148 patients remained in the study at the Week 10 time point. All patients received NUPLAZID 34 mg at Week 6 (baseline OLE) of the 10-week treatment period.8
†The 10-week treatment period includes 6 weeks of the placebo-controlled study plus the first 4 weeks of the OLE study. During the first 4 weeks of the OLE, patients and investigators remained blinded to the original treatment allocation from the placebo-controlled phase.8
Mean (SD) SAPS-PD scores at Week 6 (baseline OLE) were 12.0 (7.3) for the prior placebo group and 9.7 (7.1) for the prior NUPLAZID group.8
Mean change (SD) for the SAPS-PD score from Week 6 (OLE baseline) to Week 10 (OLE Week 4) was -3.43 (6.3) among patients who received placebo in the Phase 3 study, and -0.43 (6.8) for patients who received NUPLAZID.8
Important considerations:
-
The limitations of this study were its open‐label design and the lack of a comparison group and selection bias that could have resulted from the nonrandomized selection of patients for the OLE. However, the blinding was maintained among patients, caregivers, investigators, and remote raters.
Important Safety Information
Warnings and Precautions: QT Interval Prolongation
-
NUPLAZID prolongs the QT interval. The use of NUPLAZID should be avoided in patients with known QT prolongation or in combination with other drugs known to prolong QT interval (e.g., Class 1A antiarrhythmics, Class 3 antiarrhythmics, certain antipsychotics or antibiotics).
-
NUPLAZID should also be avoided in patients with a history of cardiac arrhythmias, as well as other circumstances that may increase the risk of the occurrence of torsade de pointes and/or sudden death, including symptomatic bradycardia, hypokalemia or hypomagnesemia, and presence of congenital prolongation of the QT interval.
Time to treatment initiation from onset of PD psychosis symptoms (post hoc analysis)
Post hoc analysis of pivotal trial: treatment response based on duration of symptoms
This post hoc responder analysis was designed to assess SAPS-PD score change in patients who started on NUPLAZID within 6 months of PD psychosis symptom onset vs patients that started NUPLAZID 6 months or later. The results of this post hoc analysis come from the pivotal Phase 3, randomized, double-blind, placebo-controlled clinical trial. A total of 95 patients who received active treatment with NUPLAZID were included in this analysis.9
Proportion of patients (responders) with SAPS-PD score improvement by time of NUPLAZID treatment initiation (N=95)9


Across all defined response thresholds, patients who started NUPLAZID within 6 months of PD psychosis symptom onset had numerically higher response rates than those who were treated later.9
Earlier vs later treatment initiation
30.8% of patients who started NUPLAZID within 6 months of PD psychosis symptom onset had a complete response on the SAPS-PD scale, compared to 11% of patients who initiated treatment after ≥6 months9
“No change or worsening” in SAPS-PD was 15.4% for early treatment vs 18.3% for later treatment9
Limitations of the post hoc analysis:
These analyses were not prespecified endpoints, they are descriptive and supportive of the clinical information related to the FDA-approved indication for the treatment of hallucinations and delusions associated with PD psychosis10
These results should be interpreted cautiously since this study has a small sample size and was not designed or powered to draw clinical conclusions, and treatment differences cannot be regarded as statistically significant10
Maintenance efficacy data (post hoc analysis)
NUPLAZID maintenance efficacy data in patients with PD psychosis with PD dementia
The results of this post hoc subgroup analysis come from a Phase 3, double-blind, placebo-controlled, randomized discontinuation study. The study included a 12-week, open-label phase followed by a 26-week, double-blind randomized phase that evaluated patients for relapse of psychosis. The study was stopped early for demonstrating positive efficacy at a preplanned Interim Analysis.11*
In the open-label phase of this study, a subgroup of patients (N=49) with PD psychosis with PD dementia receiving NUPLAZID 34 mg, 73.5% of patients met sustained response criteria† and were randomized 1:1 into the 26-week double-blind phase to continue on NUPLAZID 34 mg (N=16) or placebo (N=20).11
Lower relapse rates observed in patients taking NUPLAZID vs placebo11
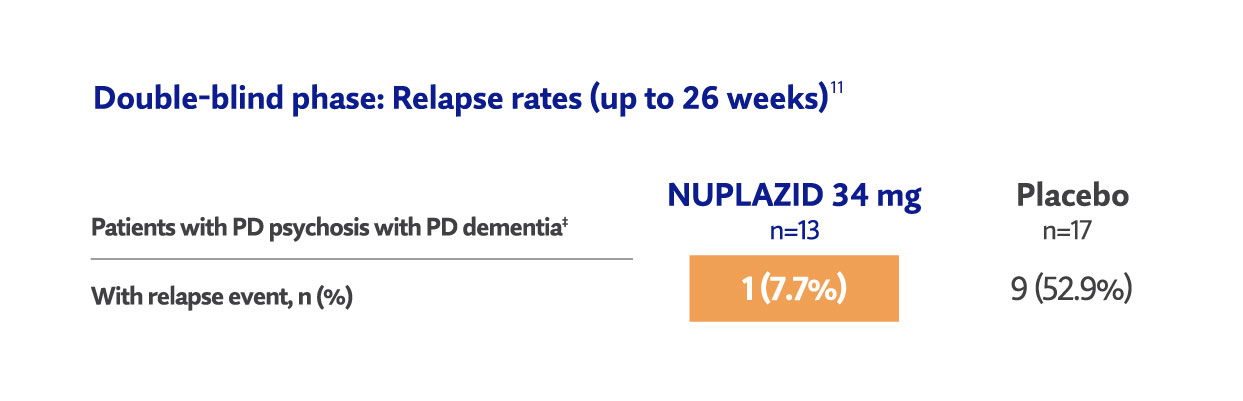
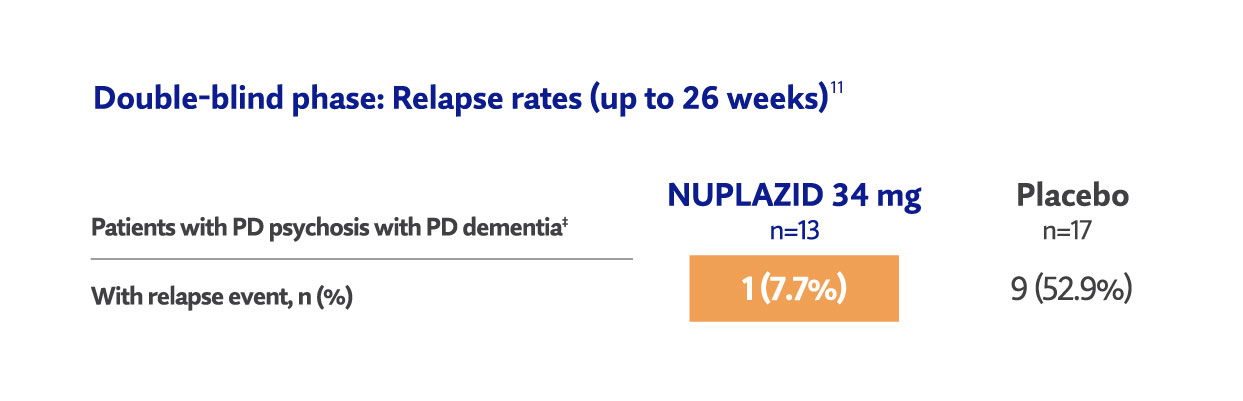
Important considerations
- The results of the post hoc subgroup analysis presented here are descriptive and supportive of the clinical information related to the FDA-approved indication for the treatment of hallucinations and delusions associated with PD psychosis
- These results should be interpreted cautiously since the study was not designed or powered to demonstrate an effect in the subgroup
*Prespecified stopping criterion required a 1-sided P value of <0.0033 at the preplanned Interim Analysis.11
†Response was defined as a ≥30% reduction (improvement) in SAPS-H+D total score and a CGI-I score of 1 (very much improved) or 2 (much improved), relative to open-label baseline, at both Weeks 8 and 12.11
‡Two patients in the placebo group and 3 patients in the NUPLAZID 34 mg group completed Week 26 of treatment without having a relapse. Other censored patients either prematurely discontinued the study prior to Week 26 for reasons not due to relapse or were ongoing in the study at the time of Interim Analysis cutoff.11
Study details
Patients experienced 1 or more of the following11:
- ≥30% increase (worsening) from Week 12 (double-blind phase) in SAPS-H+D total score and a CGI-I score of 6 (much worse) or 7 (very much worse) relative to double-blind baseline
- Treatment with another antipsychotic for symptoms of psychosis
- Drug discontinuation due to lack of efficacy
- Hospitalization for worsening symptoms of psychosis
- To be enrolled, patients:
- Had to have MMSE total scores of 6 through 2411
- Had to have symptoms of psychosis for ≥2 months and all of the following at Visit 1 (screening): SAPS H+D total score ≥10, CGI-S score ≥4 (moderately ill), and SAPS-H+D global item (H7 or D13) score ≥4 (marked)11
- Mean (SE) age of patients with PD psychosis with PD dementia was 72.6 (1.08) years prior to initiation of open-label drug administration. Mean (SE) MMSE score in patients with PD psychosis with PD dementia was 18.9 (0.74) at open-label baseline11
- 44.9% (22/49) of patients took anti-dementia medications during the open-label phase11§
§Patients who were on concomitant anti-dementia therapy took at least 1 anti-dementia medication such as donepezil, memantine, and/or rivastigmine. Patients who were receiving an anticholinesterase inhibitor, memantine, or both had to be receiving a stable dose for 12 weeks before screening.10
CGI-I=Clinical Global Impression-Improvement scale; CGI-S=Clinical Global Impression-Severity scale; MMSE=Mini-Mental State Examination; SAPS-H+D=Scale for the Assessment of Positive Symptoms-Hallucinations and Delusions; SE=standard error.
Important Safety Information
WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS
-
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death.
-
NUPLAZID is not approved for the treatment of patients with dementia who experience psychosis unless their hallucinations and delusions are related to Parkinson’s disease.
Learn about the demonstrated safety of NUPLAZID.
Acadia Connect® provides comprehensive prescription support.
 IMPORTANT SAFETY INFORMATION and INDICATION
IMPORTANT SAFETY INFORMATION and INDICATION
WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS
- Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death.
- NUPLAZID is not approved for the treatment of patients with dementia who experience psychosis unless their hallucinations and delusions are related to Parkinson’s disease.
- Contraindication: NUPLAZID is contraindicated in patients with a history of a hypersensitivity reaction to pimavanserin or any of its components. Rash, urticaria, and reactions consistent with angioedema (e.g., tongue swelling, circumoral edema, throat tightness, and dyspnea) have been reported.
-
Warnings and Precautions: QT Interval Prolongation
-
NUPLAZID prolongs the QT interval. The use of NUPLAZID should be avoided in patients with known QT prolongation or in combination with other drugs known to prolong QT interval (e.g., Class 1A antiarrhythmics, Class 3 antiarrhythmics, certain antipsychotics or antibiotics).
-
NUPLAZID should also be avoided in patients with a history of cardiac arrhythmias, as well as other circumstances that may increase the risk of the occurrence of torsade de pointes and/or sudden death, including symptomatic bradycardia, hypokalemia or hypomagnesemia, and presence of congenital prolongation of the QT interval.
-
- Adverse Reactions: The adverse reactions (≥2% for NUPLAZID and greater than placebo) were peripheral edema (7% vs 2%), nausea (7% vs 4%), confusional state (6% vs 3%), hallucination (5% vs 3%), constipation (4% vs 3%), and gait disturbance (2% vs <1%).
-
Drug Interactions:
-
Coadministration with strong CYP3A4 inhibitors increases NUPLAZID exposure. Reduce NUPLAZID dose to 10 mg taken orally as one tablet once daily.
-
Coadministration with strong or moderate CYP3A4 inducers reduces NUPLAZID exposure. Avoid concomitant use of strong or moderate CYP3A4 inducers with NUPLAZID.
-
Indication NUPLAZID is indicated for the treatment of hallucinations and delusions associated with Parkinson’s disease psychosis.
Dosage and Administration Recommended dose: 34 mg capsule taken orally once daily, without titration, with or without food.
NUPLAZID is available as 34 mg capsules and 10 mg tablets.
Please read the full Prescribing Information, including Boxed WARNING.
References:
- Acadia Pharmaceuticals Inc. NUPLAZID® [package insert]. San Diego, CA; 2023.
- Cummings J, Isaacson S, Mills R, et al. Pimavanserin for patients with Parkinson’s disease psychosis: a randomised, placebo-controlled phase 3 trial. Lancet. 2014;383(9916):533-540.
- Data on File_ACP-103-020 posthoc demographics_ July2020.
- Espay AJ, Guskey MT, Norton C, et al. Pimavanserin for Parkinson’s disease psychosis: effects stratified by baseline cognition and use of cognitive-enhancing medications. Mov Disord. 2018;33(11):1769-1776.
- Voss T, Bahr D, Cummings J, Mills R, Ravina B, Williams H. Performance of a shortened scale for assessment of positive symptoms for Parkinson’s disease psychosis. Parkinsonism Relat Disord. 2013;19(3):295-299.
- Andreasen NC. Scale for the Assessment of Positive Symptoms (SAPS). Iowa City, IA: University of Iowa; 1984.
- Fahn S, Elton R, Members of the UPDRS Development Committee. Unified Parkinson’s Disease Rating Scale. In: Fahn S, Marsden CD, Calne DB, Goldstein M, eds. Recent Developments in Parkinson’s Disease. Vol 2. Florham Park, NJ: Macmillan Health Care Information; 1987:153-163, 293-304.
- Isaacson SH, Coate B, Norton J, Stankovic S. Blinded SAPS-PD assessment after 10 weeks of pimavanserin treatment for Parkinson's disease psychosis. J Parkinsons Dis. 2020;10(4):1389-1396. doi:10.3233/JPD-202047
- Data on file. 2025.
- Data on File. Post-hoc analysis limitations. 2025.
- Data on file. ACP-103-045_PDD 34 mg subgroup_Sep2021.



